Contact
Contact
Gavra Vukovića b.b, Podgorica
Dentistry: 020 227 227
Polyclinic: 020 227 224
Gynecology: 020 227 444
Segova Program is the most advanced, innovative and safest autologous method of organic regeneration of the gonads, preformed at Specialized hospital Ars Medica by Prof dr Aleksandar Ljubic.
It requires the use of patients own cells and growth factors in order to re-establish and improve the function of gonads and the production of hormons, improving in this way both reproductive health and the overall body functions.
This program regenerates the function of ovaries, helps delay menopause, and prevents age related pathologies.
The main advantage of SEGOVA is based on autologous, organic regeneration of the gonads, the organs which change the most through ageing. Gonads, ovaries and testes, influence the functioning and structure of all other tissues and organs within the organism.
Restoration of normal gonadal function – production of oocytes/eggs or sperm cells, necessary for reproduction and hormones, essential for the proper function of the whole body, depends on a variety of elements.
The gonads must contain adequate cells which are to be developed into eggs and sperm. These organs also produce hormones, assuming the existence of adequate control mechanisms (mostly growth factors) and the right amount of energy for these demanding processes which are controlled by very strict genetic mechanisms.
Ovarian rejuvenation technology is aimed at counteracting age-related fertility decline and its concomitant complications, as well as decline in ovarian function caused by pathological conditions. Ovarian tissue re-implantation as potential therapy and oocyte banking for anticipated gamete exhaustion has been proposed in such cases.

CANDIDATES
Age-related ovarian dysfunction and fertility decline in women has emerged as an indication for ovarian rejuvenation as the age at which women now attempt their first pregnancy has been steadily rising over the last decades. Female fertility naturally decreases significantly after the age of 35 years, causing poor oocyte quality, abnormalities in the meiotic spindle, chromosome misalignment and shortened telomeres.
There are different groups of women seeking fertility preservation or ovarian rejuvenation, including patients with the hematological malignancies, women with premature ovarian failure and infertility as well as those who wish to postpone childbearing for various personal reasons, with age becoming the main threat to their fertility.
Following the SEGOVA procedure, restored ovarian tissue takes over the role that it had before and begins the production of its own sex hormones. The lost functions of the ovaries are re-established and all other organs and tissues in the body are rejuvenated and their work is improved.
PROCEDURE
SEGOVA Program consists of several separate procedures integrated in a common project aimed to support, increase or create elements necessary for normal gonadal function.
The first letters of the SEGOVA abbreviation in fact represent the specific procedures:
S – Stem cell therapy
Cell therapy which uses autologous stem cells – cells obtained from the patients’ own body. The aim is to create new or incite existing non-differentiated gonadal stem cells – which are to be developed into new oocytes or sperm cells and the hormone-producing cells.
E – Energy mitochondrial boosting
Stem cell therapy is correcting mitochondrial function in existing cells However, boosting mitochondrial energy production in gonadal cells with a specific physical exercise regime – HIIT (High Intensity Interval Training) is a combination of highly intensive, intermittent, specific anaerobic exercise.
G – Growth factor PLPR therapy
Growth factors are essential mediators in gonadal control mechanisms. These growth factors are obtained from the patient’s own blood and used to treat gonadal tissue. They act by controlling the creation and growth of eggs and the surrounding cells responsible for hormone production. In recent years, ovarian revitalization methods have been applied worldwide in order to improve the hormonal and reproductive conditions of the patient and thus their quality of life. PLRP is a separated part of the whole blood where the high platelet level is concentrated, but with growth factors of 3 to 5 times the plasma concentration. Growth factors are found in the granules and they play an important role in cell proliferation, chemotaxis, promotion of angiogenesis and differentiation of mesenchymal and other types of cells.
OVA – Ovarian in Vitro Activation
The production of eggs – oogenesis, is dependent on proper genetic control. Hippo the signaling pathway is essential for maintaining optimum organ size. It contains several negative growth regulators. The AKT the signaling pathway has a key role in the initiation of follicle growth. The ovarian in vitro activation represents the autologous genetic treatment of the gonadal tissue in order to restore both reproductive and endocrine functions of the ovary.
PROCEDURE BY DAYS:
SEGOVA procedure day 0
Arrival to your selected SEGOVA Program clinic and time with nutritional and physical specialists.
SEGOVA procedure day 1
The SEGOVA procedure begins by taking the patient’s blood, from which the cells rich in growth factors are separated and prepared for activation. This is followed by a gonadal biopsy performed using a minimally invasive procedure under local or general anesthesia. The obtained gonadal tissue is micro fragmented.
SEGOVA procedure day 2
A resting day for the patient at the hospital. Meanwhile the tissue particles are being incubated in growth factors from previously obtained blood cells. It is done in a specifically controlled conditions in a laboratory.
SEGOVA procedure day 3
This phase requires bone marrow sampling by performing the puncture of the shinbone. Bone marrow is processed to separate the patients stem cells. The ultrasound 4D the color guided needle gonadal re-transplantation is used to insert previously processed gonadal tissue with growth factors. The same approach is for the next step – stem cells application into the gonads. Following this the patient is discharged from the clinic the same afternoon and able to return to their regular activities or travel.

SEGOVA FOR MEN
The age-related decline in testosterone along with the associated symptoms has been referred to as male menopause or the andropause. Partial androgen deficiency and the decline in testosterone seen in ageing men has clinical implications. Along with the decline in testosterone, some men experience symptoms that include: fatigue, weakness, depression, sexual dysfunction. Standard medical therapy today – Testosterone replacement is connected with potential risks and side effects.
SEGOVA Program for men follows the standard set of SEGOVA procedures and includes the standard follow up program.

FOLLOW UP PROGRAM
SEGOVA Program follow up begins at the end of the SEGOVA procedure completion. We provide test results upon your departure and following the first month of the procedure we as you to perform certain blood work tests and share the results with us. Usually the same, sometimes additional, tests are then performed at quarterly intervals during the period of up to two years if not otherwise requested by SEGOVA medical team and agreed with the patient.

SEGOVA + SEGO + PRP PATIENTS
- The sample of 93 patients, aged 31 – 60 , (average value 46,64) diagnosed with infertility completed the Segova program and participated In one year long follow up.
- The sample of 93 patinets had sonographic and hormone level (FSH, LH, E2, PG, AMH) follow up throughout the course of one year since the procedure.
- The study was conducted at the Specialized OBGYN hospital Jevremova Belgrade, Saint James Hospital in Malta, Remedica Hospital in Skopje, from 2015 to 2019.
- All the patients have undergone preparatory laboratory analysis and completed the questionnaires about menstrual cycles, parity, presence of POF-a diagnosis in family history, education level and possible sources of stress prior to amenorrhea. Questionnaires concerning life quality were also completed.
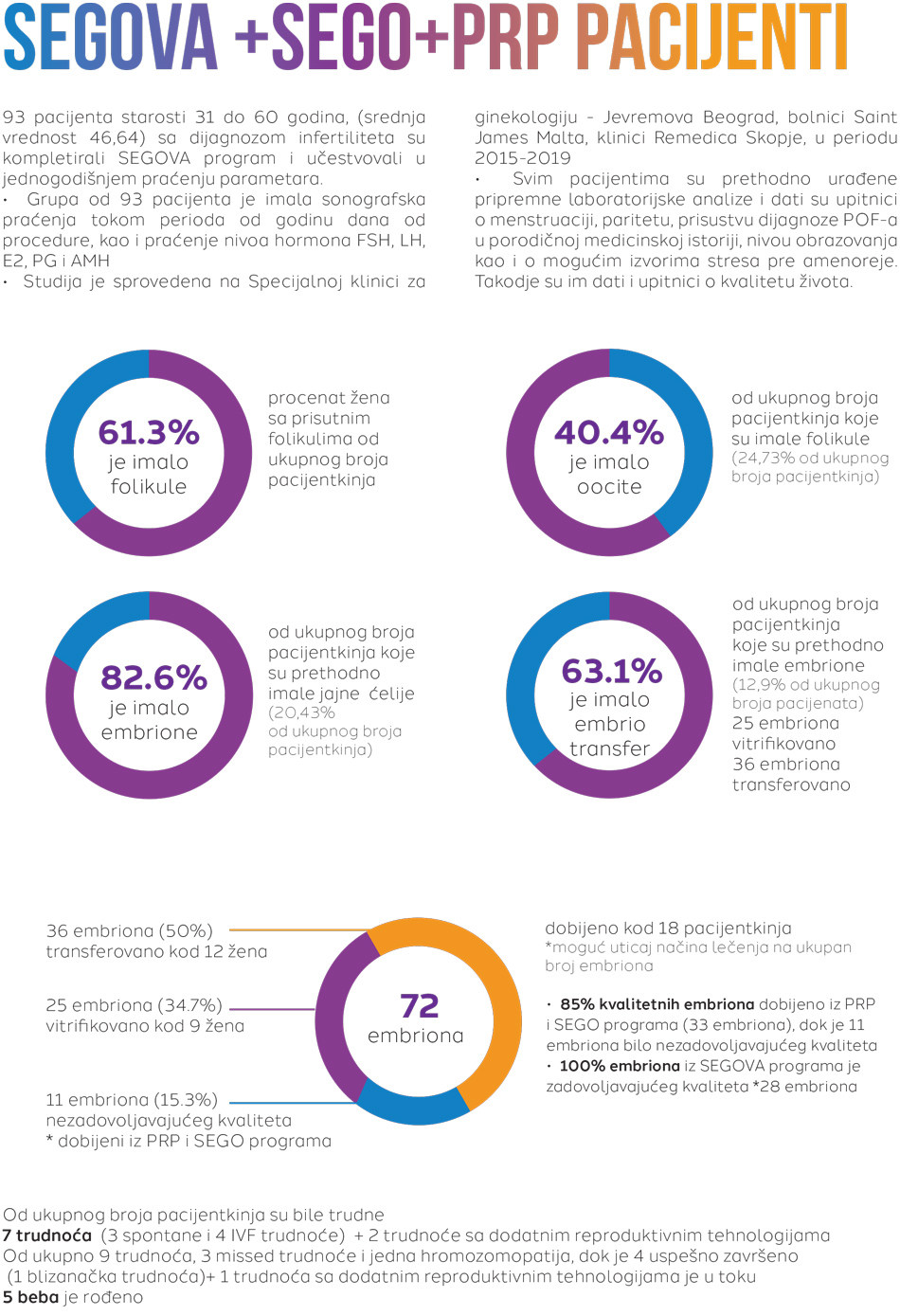

From the total number of patients, 7 patients were pregnant (3 spontaneous and 4 IVF pregnancies) + 2 pregnancies with additional reproductive technologies.
From 9 pregnancies in total – 3 missed pregnancies, 1 chromosomopathy, and 4 succesfull pregnancies ( one twin pregnancy + one pregnancy with additional reproductive technologies currently In progress = total of 5 babies were born)
Nakon specijalističkog pregleda se pristupa neophodnim pretragama i analizama, koje pacijenti mogu obaviti u okviru naše bolnice.
Pošaljite zahtjev
prof dr Aleksandar Ljubić

Aleksandar Ljubić rođen je 1958. godiine u Beogradu, gdje je završio školovanje, postdiplomske, magistarske i doktorske studije. Svoje profesionalno usavršavanje nastavio je u SAD-u, Japanu, Velikoj Britaniji i Italiji.
Radno iskustvo:
2015 – Zamjenik Generalnog sekretara Svjetske asocijacije za perinatalnu medicinu;
2013 – 2014 Medicinski direktor Medigroup-e;
2009 – Predsjednik Upravnog odbora Klinike za dječiju neurologiju;
1995 – 2013 Medicinski fakultet u Beogradu, kao asistent, docent, potom i vanredni profesor ginekologije i akušerstva;
Profesor je i na DIU (Dubrovnik International University);
2004 – 2013 Klinički Centar Srbije, prvo kao pomoćnik direktora, potom i kao direktor Klinike za Ginekologiju i akušerstvo;
1986 – 2013 Klinika za ginekologiju i akušerstvo, Klinički centar Srbije; 13 godina načelnik odeljenja carskih rezova i visokorizičnih trudnoća.
Reference / stručnu radovi / članstva:
Rukovodilac 10 međunarodnih i nacionalnih naučnih projekata i autor preko 450 članaka i 25 knjiga;
Član uredništva u 6 stručnih časopisa;
Potpredsjednik stručnog savjeta Kliničkog Centra i koordinator izgradnje nacionalnog biotehnološkog centra;
Predsjednik Udruženja za ultrazvuk Srbije, osnivač i prvi direktor srpske grane internacionalne škole za ultrazvuk “Ian Donald”;
Dugogodišnji predsjednik Republičke komisije za vantelesno oplođenje i potpredsjednik Republičke komisije za perinatalnu medicinu;
Član međuodeljenskog odbora SANU za humanu reprodukciju.


